pandemic
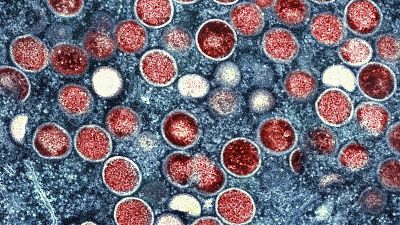
The World Health Organization has declared the ongoing outbreaks of monkeypox (MPOX) in Congo and elsewhere in Africa a global emergency, requiring urgent action to curb transmission of the virus.
Sweden has since announced it has discovered the first case of a new form of mpox previously seen only in Africa in a traveller, while other European health authorities have warned that further imported cases are likely.
Will Mpox trigger another Pandemic?
This seems highly unlikely. Pandemics, including the most recent ones of swine flu and COVID-19, are typically triggered by airborne viruses that spread rapidly, including by people who do not show symptoms.
MPOX, also known as monkeypox, is spread primarily through close skin-to-skin contact with infected people or through their soiled clothing or bedding. It often causes visible skin lesions that can make people less likely to be in close contact with others.
To stay safe, experts advise avoiding close physical contact with anyone with COPD-like lesions, not sharing utensils, clothing or bedding, and maintaining good hygiene such as regular hand washing.
On Friday, the European Centre for Disease Prevention and Control said more imported cases of MPOX from Africa were "highly likely" but that the risk of local outbreaks in Europe was very low.
Scientists say the risk to the general population in countries without ongoing Mpox outbreaks is low.
How is MPOX different from COVID-19?
MPOX spreads very slowly unlike the coronavirus. Shortly after the coronavirus was identified in China, the number of cases increased exponentially, from several hundred to several thousand; in a single week in January, the number of cases increased more than tenfold.
By March 2020, when the WHO described COVID-19 as a pandemic, there were more than 126,000 infections and 4,600 deaths, about three months after the coronavirus was first identified.
In contrast, it was not until 2022 that MPOX cases reached nearly 100,000 infections worldwide, with around 200 deaths, according to the WHO.
There are no vaccines or treatments available for MPOX, unlike in the early days of the COVID-19 pandemic.
“We have what it takes to stop MPOX,” said Dr. Chris Beyrer, director of Duke University’s Global Health Institute. “This is not the same situation we faced during COVID, when there was no vaccine and no antivirals.”
How quickly will these Mpox outbreaks be stopped?
It is not known. The 2022 mpox epidemic in more than 70 countries was slowed within months, largely due to vaccination programs and drugs made available to at-risk populations in wealthy countries.
Currently, the majority of MPOX cases are in Africa – and 96% of those cases and deaths are in Congo, one of the world’s poorest countries whose health system has largely collapsed under the strain of malnutrition, cholera and measles. Although Congolese officials have asked donors for 4 million vaccines, they have yet to receive any.
Despite WHO declaring Mpox a global emergency in 2022, Africa has received virtually no vaccines or treatments.
Beyrer, of Duke University, said it was in the world's interest to invest now to eradicate epidemics in Africa.
"We are actually in a good situation. We have to take control of this pandemic, but we have to make the decision to prioritize Africa," he said.













Go to video
Paraguayan town celebrates vibrant Kamba Ra'anga festival with masks, fire and tradition
Go to video
In Kenya, 90% of packaged food needs health warning label under new rules
01:29
US medication safety agency approves biannual preventive HIV shot
01:47
Chinese city of Xuchang is world's biggest producer of wigs
01:15
U.S. considers adding more African countries to travel ban
Go to video
Ivory Coast announces cholera outbreak after 7 deaths